Plantar Fasciitis or Baxter’s Entrapment ?
Some cases of Plantar Fasciitis may actually be Baxter’s Entrapment.
In fact, the clinical picture may of Baxter’s Entrapment and Plantar Fasciitis can be virtually identical.
Baxter’s neuropathy may account for up to 20% of heel pain cases,1,2 although it is frequently misdiagnosed. If it is misdiagnosed as Plantar Fasciitis then traditional Plantar Fasciitis treatments could be ineffective, or actually make the condition worse.
What is Baxter’s Entrapment or Baxter’s Neuropathy?
Baxter’s Entrapment is an entrapment (or compression) of the Inferior Calcaneal Nerve just under the base of the arch of the foot. The Inferior Calcaneal Nerve is the first branch of the Lateral Plantar Nerve on the bottom surface of the foot. The nerve is also sometimes called Baxter’s nerve, named after the first physician to describe this nerve entrapment as a specific cause of foot pain.
Risk Factors:
- Plantar Fasciitis
- Obesity
- Flat Foot
- Foot Hyperpronation
- Muscular Enlargement (such as in athletes)
- Bone Spur (Plantar Calcaneal Spur)
Unsure if You Have Baxter’s Entrapment or Plantar Fasciitis?
Get Help Now:
It is difficult to identify compression of the Inferior Calcaneal nerve with physical examination. Frequently, it is painful to feel along the arch on the bottom surface of the foot. In some cases it will be especially painful to feel along the outer aspect of the bottom of the foot where the Abductor Digiti Minimi muscle is located. It may also be painful along the inner arch where the nerve is likely to be entrapped.
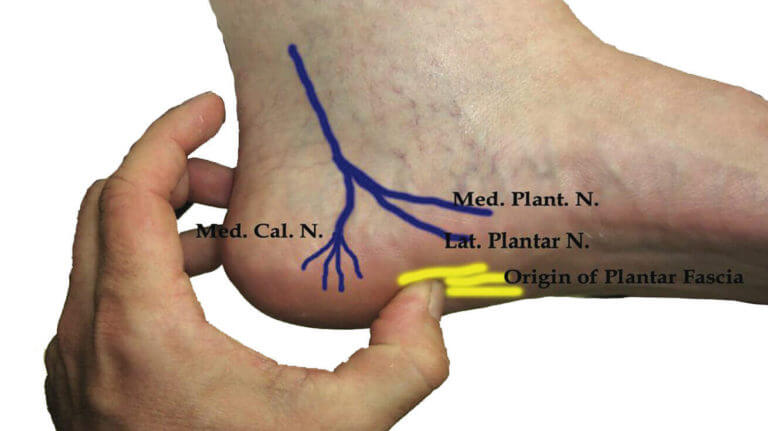
It is very difficult to identify the clinical indicators of inferior calcaneal nerve compression through physical examination, so this nerve compression is often missed unless an ultrasound guided local anesthetic diagnostic test or MRI is performed. A local anesthetic agent (such as lodocaine) is injected near the origin of the Medial Calcaneal Nerve using ultrasound guidance to increase accuracy. If the trial injection results in a significant decrease in pain, then this indicates that Baxter’s Entrapment is likely to be present.
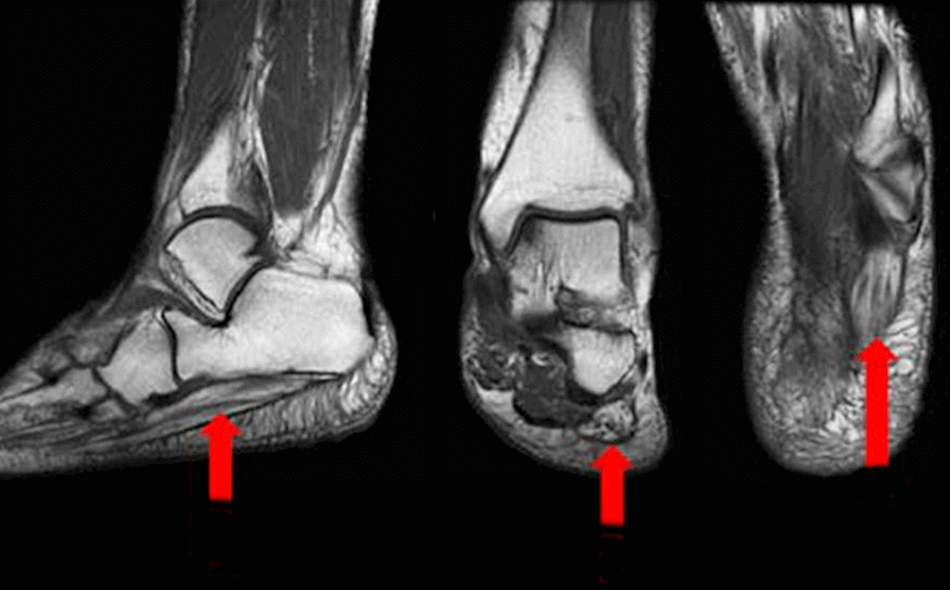
MRI
MRI has been shown to be valuable in demonstrating muscular changes associated with denervation. When motor fibers to the abductor digiti minimi muscle are damaged, the muscle will atrophy and fatty edema can build up in the muscle. The fatty infiltration of muscle is visible on the MRI. MRI is also helpful in excluding alternative diagnoses (fracture, neoplasia, fasciitis).
Treatment
Ultrasound guided Radiofrequency Ablation
Ultrasound guided radiofrequency ablation is a high-level procedure for Baxter’s Entrapment that can produce long-term pain relief and has high patient satisfaction scores. It is a minimally invasive intervention that uses high frequency sound waves to heat the affected sensory nerve to 90 degrees Celsius.
Proteins in the nerve are broken down at this temperature and the targeted section of the nerve is destroyed. This prevents the nerve fibers from transmitting pain from that area. Additionally, radiofrequency ablation may cause the formation of new blood vessels, thereby accelerating the healing process. At our center, this minimally invasive procedure is performed under local anesthesia and with ultrasound guidance to ensure an accurate targeting.
The Procedure

Radiofrequency ablation is generally painfree. You are likely to feel pain only when the local anesthetic is injected into the target area in the foot before the procedure. After the skin is anesthetized, a very small puncture is made over the painful zone. The radiofrequency ablation needle is introduced using ultrasound to guide its positioning. The accurate position of the needle is then rechecked and may be adjusted using a nerve stimulator. Once the needle is in the precise position, an electrode is placed through the needle. The tip of the electrode is then heated to around 90 degrees Celsius for a short period. The procedure is repeated according to protocol. The treated area is protected with a bandage and the patient is advised to reduce activity, and to ice and elevate the foot for the rest of the day. The bandage can be removed the following day and the patient can then use a regular Band-Aid to cover the treated area. You should keep the treated area dry and clean for at least 24 hours. Normal activity can be resumed in one or two days. Any pain that may occur can be managed with an NSAID or Tylenol.
What to expect after Radiofrequency Ablation
This procedure does not usually cause side effects, but a few are possible. You may develop bruising at the puncture site that can cause pain. Numbness or a lack of sensation around the puncture area can also occur, but this side effect is rare. Abscess formation or infections at the incision site are rare.
You should experience relief from this procedure within a week, but it may take longer to fully heal. In the 2 months following the procedure, we recommend regular stretching and a continued use of heel pads or arch supports. You should be able to resume physical activities such as jogging or other sports one month after the intervention. If pain is still present after four to six weeks, radiofrequency ablation can be performed again. If none of these procedures improve the pain, you may need to consider other invasive procedures. The majority of patients report a significant decrease in pain after two radiofrequency ablations.
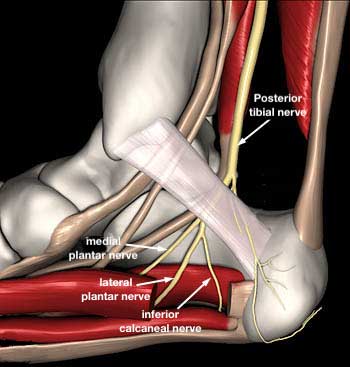
Anatomy
The Posterior Tibial Nerve divides into two primary branches, the Medial and the Lateral Plantar Nerves, in the tarsal tunnel as it passes around the medial side of the ankle. Both branches then curve around the medial ankle and course along the bottom surface of the foot.
The Medial Plantar Nerve travels anterior to the Lateral Plantar Nerve, carrying sensory information from the medial two thirds of the plantar foot, and motor innervation to the flexor digitorum brevis, abductor hallucis, flexor hallucis brevis, and first lumbrical.
The Lateral Plantar Nerve carries sensory information from the lateral plantar aspect of the foot, 5th toe, and lateral half of the 4th toe. Motor innervation involves all the remaining foot muscles, not innervated by the Medial Plantar Nerve.
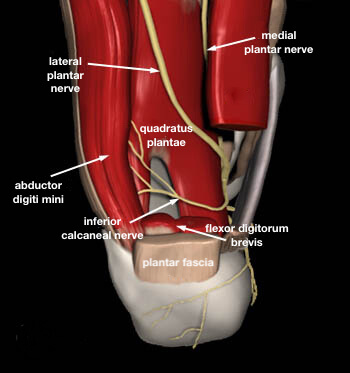
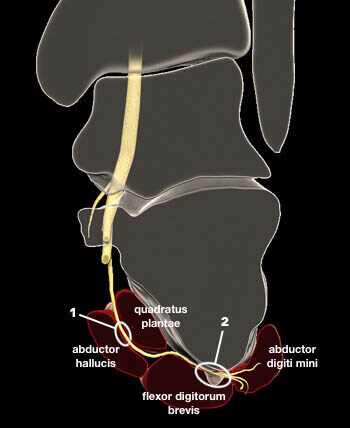
The first branch that splits off from the Lateral Plantar Nerve is known as the Inferior Calcaneal Nerve or Baxter’s Nerve. It is a mixed sensory and motor nerve, providing motor innervation to the abductor digiti minimi muscle. Weakness of this muscle may be present but is difficult to detect clinically. The Inferior Calcaneal Nerve originates from the Lateral Plantar Nerve at various levels beneath the deep fascia of the abductor hallucis muscle. In most people, the Inferior Calcaneal Nerve branch splits off from the Lateral Plantar Nerve on the underside of the foot. However, in some cases the Inferior Calcaneal Nerve may actually branch off more proximally, even as far up as the tarsal tunnel on the medial ankle. Rarely, the nerve can originate directly from the Posterior Tibial Nerve. The nerve courses vertically between the abductor hallucis and quadratus plantae muscles, then makes a sharp 90 degree horizontal turn, coursing laterally beneath the calcaneus to innervate the abductor digiti minimi muscle.
Where and how a nerve splits is relevant because of the compressive loads on the nerve which may lead to nerve injury. Another important factor is the sharp right angle turn the nerve takes from the medial side of the foot to the plantar surface.
The Inferior Calcaneal Nerve supplies motor innervation to the abductor digiti minimi muscle, occasionally to the flexor digitorum brevis and lateral half of the quadratus plantae. Sensory information is carried from the calcaneal periosteum, long plantar ligament, and adjacent vessels.
Nerve Entrapment
Nerve entrapment can occur in 1 of 2 locations:
- Between the deep fascia of the Abductor Hallucis muscle and the the medial plantar margin of Quadratus Plantae muscle; or,
- Along the anterior aspect of the Medial Calcaneal Tuberosity where the nerve can be compressed against the bone or bone spurs that may have developed along the Anterior Calcaneus bone.
- Chundru U, Liebeskind A, Seidelmann F, Fogel J, Franklin P, Beltran J. Plantar fasciitis and calcaneal spur formation are associated with abductor digiti minimi atrophy on MRI of the foot. Skeletal Radiol. 2008;37(6):505-510.
- Pecina M, Markiewitz A, Krmpotic-Nemanic J. Tunnel Syndromes: Peripheral Nerve Compression Syndromes. Boca Raton: CRC Press; 2001.