Surgical Treatment for Plantar Fasciitis
Most patients respond to conservative treatments for Plantar Fasciitis. However, despite optimal care, about 20 to 30% of the Plantar Fasciitis patients develop chronic disease and disabling symptoms that may warrant more aggressive remedies for long-term relief. The majority of these respond to ultrasound procedures for chronic plantar fasciitis. However a small percentage of these people do not respond well. Surgery should only then be considered. Surgical intervention is usually adopted as a last resort. In less than 10% of the cases, when no other way of care seems to work and symptoms are persistent. It is critical that Plantar Fasciitis surgery should be performed by surgeons who have considerable expertise and experience in this surgery. Because, in some cases, Plantar Fasciitis surgery can result in foot instability and increased foot pain. Furthermore, there is little consensus regarding the most appropriate surgical approach that should be adopted as the ‘gold standard procedure’.
Should you have Plantar Fasciitis surgery?
A lot of patients wonder if plantar fasciitis surgery is appropriate for them. We generally advise against surgery as a treatment for plantar fasciitis symptoms for a number of reasons:
- Long recovery. The post-surgical recovery and rehabilitation period is fairly long. Most surgical candidates are unable to resume their normal daily activities for at least 6 weeks after the procedure and can only fully resume their activities after 10-12 weeks. The mean duration of rehabilitation and maximal pain improvement after endoscopic or open plantar fascial release is 1 year.
- Poor patient satisfaction. Several studies have shown that less than 50% patients report complete satisfaction after the surgical intervention. A fair chunk of surgical candidates continue to experience disabling pain and functional limitations even after the surgery.
- Foot instability. Biomechanical studies have shown that surgical release of the plantar fascia has detrimental effects on other ligamentous and bony structures in the foot. In fact, in poorly addressed situations, recurrence of plantar fasciitis is observed in over 40% cases.
- Complications. The risk of an adverse outcome after surgical procedure is fairly high. Post plantar fasciitis surgery complicationsinclude forefoot stress fractures, calcaneal and cuboid fractures, and inner or outer foot pain.


Surgical Risks and Complications
Regardless of the expertise of surgeon and utilization of best techniques, almost all operative procedures are associated with some degree of side effects or complications.
- Post-operative Scarring of Planta Fascia: A number of studies indicated that post-procedure scarring is fairly common (regardless of the nature of surgical approach). The risk of painful scarring can be minimized by using precise incisions along the lines of minimal skin tension. Although, painful scarring resolves spontaneously, some patients may require scar excision procedure to resolve persistent pain.
- Complete tearing of Plantar Fascia: Post-surgical tearing or complete severing of plantar fascia is also a likely possibility in some patients.
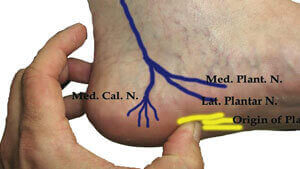
- Neuritis/ Nerve Entrapment: Patients also experience nerve pain due to neuritis or nerve entrapment (especially of Baxter’s nerve) due to abnormal scar formation. Such patients may require nerve excision or nerve release procedures for early return to normal day-to-day operations.
- Fibrosis/ Reattachment of fibers: Likewise, inadequate or insufficient release of plantar fascia may lead to fibrosis and reattachment of fibers to cause persistent pain and discomfort. Other causes of pain include; inflammatory reaction due to procedure or metabolic causes of recalcitrant pain; such as ankylosing spondylitis, reactive arthritis, psoriatic arthritis, gout, SLE, rheumatoid arthritis, and inflammatory bowel disease.
- Instability: Temporary instability is usually a result of a temporary changes in the biomechanics of foot support. In most cases, supporting structures of the foot (such as muscles, tendons and ligaments) adapt to the new role.
- Stress fractures: The instability of lateral column instability exert more pressure and pull on the surrounding structures. Most patients experience fatigue, and strain that may culminate in stress fractures.
- Other. Less frequently reported complications are; transient swelling of the heel, medial arch pain, sinus tarsitis, pain in the metatarsal region, compartment syndrome, posterior tibial nerve damage, flattening of longitudinal arches and hypoesthesia of heel.
We recommend opting for conservative options as well as non-urgical interventions to resolve the symptoms of plantar fasciitis.
Types of Surgical Procedures:
The most common surgical procedure for plantar fasciitis is fasciotomy – the release of the plantar fascia to decrease the tension in the foot musculature. This can be done with or without removal of heel spurs. Endoscopic plantar fasciotomy is becoming more popular due to its faster recovery time.
The surgical approach is dependent upon the surgeon’s preference, anatomical and pathological factors, patient factors and goals of the surgery. In most cases the primary aim of surgery is to lengthen the plantar fascia ligament. Sometimes, when plantar fasciitis is associated with a heel spur, the secondary goal of the surgery is spur removal in order to minimize the risk of recurrence.
 Heel spurs are quite common even in the general population and are usually not associated with any symptoms of discomfort or inflammation. The decisions regarding to surgical approach and remove heel spur is dependent on:
Heel spurs are quite common even in the general population and are usually not associated with any symptoms of discomfort or inflammation. The decisions regarding to surgical approach and remove heel spur is dependent on:
- Size of the heel spur
- Anatomical alignment or positioning of spur (backward facing or forward facing)
- Location of the heel spur
- Co-existing condition of the foot and severity/ nature of symptoms.
Fascial release and resection:
There is little consensus regarding the actual quantity of fascial release and resection. Most surgeons advocate the release of only the medial 1/3 rd of the plantar fascia due to minimal risk of lateral column destabilization. Other surgeons believe that release of medial 2/3 rd’s of plantar fascia minimizes the risk of recurrence. It is safe to assume that different patients require different approaches.
The most common surgical approaches are
Open plantar fasciotomy

Several factors are considered while performing open plantar fasciotomy; such as incision placement, release of plantar fascia and post-release stabilization. Traditional open plantar release can be performed by multiple approaches.
Plantar (bottom of the foot) incision is the most preferred approach in chronic cases as it gives maximum visualization of the plantar ligaments and associated structures such as heel spur.
If plantar fascia is thick and diseased, use of in-step plantar approach (a variant of traditional plantar approach) helps in facilitating selective release of the plantar fascia and speedy post-operative healing. In addition, this approach is also associated with minimal risk of adverse effects and long-term complications. However, immediate post-operative weight bearing should be avoided to allow maximal healing to plantar incision.
Another open plantar release is the Medial plantar fasciotomy. In this surgical approach, the surgeon access plantar fascia from the inside of the main arch (proximal medial arch ) of the foot. As part of the procedure, the surgeon performs ligament release after feeling the anatomy and alignment of structures; which is then followed by blind excision of the plantar fascia. Although this surgical approach is less invasive and has a faster recovery, the risk of complications is slightly higher. The expertise of your surgeon can greatly determine the operative outcomes in medial plantar fascia release.
Endoscopic plantar fasciotomy

Endoscopic plantar fasciotomy (or endoscopic plantar fascia release) is a relatively new procedure that is associated with minimal surgical dissection of the tissue with the help of delicate instrumentation and precise tissue resection. The surgical resection of plantar fascia is always performed under direct visualization via endoscopic cameras.
The key features of endoscopic fasciotomy vs. an open approach are:
- Relatively faster rehabilitation period and overall shorter recovery period;
- Patients can expect early return to normal functioning; and,
- Immediate post-procedure weight- bearing
Endoscopic fasciotomy procedures are associated with high quality post-operative results. The success rate by endoscopic approach is about 80-90%. Patients who undergo endoscopic plantar fascial release report good improvement in their symptoms after the initial rehabilitation period.
Aside from the faster recovery, the long-term outcomes of endoscopic plantar fascia release are mostly similar to open fasciotomy in terms of nerve entrapment and persistent pain.
Other surgeries for plantar fasciitis – Proximal Medial Gastrocnemius Release:
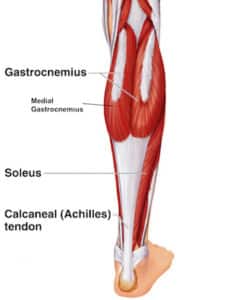
Depending upon the pathophysiology and other patient factors, other surgical procedures can also be attempted such as proximal medial gastrocnemius release (also referred to as PMGR). A fair chunk of plantar fasciitis patients have isolated rigidity or tightness of gastrocnemius muscle which significantly impairs the bio-mechanics of the lower limb (both knee and ankle joint); leading to limited ankle movement (coupled with altered knee extension). This surgical procedure is especially helpful in these patients to minimize the risk of recurrence of plantar fasciitis. Patient satisfaction scores are quite high with PMGR (more than 95%) and most patients are able to resume their normal day-to-day operations within 3 weeks after the procedure.