Diagnosis of Plantar Fasciitis
First and foremost, the diagnosis of plantar fasciitis is a clinical one. Further investigations should be tailored depending on the clinical picture. Care should be taken when diagnosing foot conditions like plantar fasciitis. It is best to consult with an experienced practitioner for prompt diagnosis since early treatment is the key to reduce the risk of complications.
The vast majority of folks suffering from plantar fasciitis will have moderate heel pain and discomfort; however, some people may have generalized pain and tenderness on the sloes of their feet. It is important to keep in mind that a number of foot conditions can mimic plantar fasciitis and therefore seeing an experienced provider is critical.
Don’t Suffer Any More…
Do you have Baxter’s Entrapment?
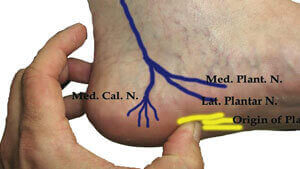
Baxter’s entrapment can be just like Plantar Fasciitis. In fact, clinically it can be impossible to tell them apart. The only way to tell them apart is by an ultrasound guided diagnostic injection. Yet the treatments are completely different. Baxter’s Entrapment should be treated by an ultrasound guided ablation procedure.
Clinical History
The clinical history and physical examination is key in diagnosing plantar fasciitis. The most important features of the clinical history are morning stiffness and aggravation of pain on bending the foot upwards (dorsiflexion), which occurs in activities like standing on your toes or walking up stairs. The location of the pain is important in making the correct diagnosis. Plantar fasciitis pain is typically localized on the inside of the heel which is where the plantar fascia attaches. In some cases, tenderness may occur on the long arch of the foot or even the sole of the foot. Your doctor may squeeze or press on the inside of your heel to reproduce the pain and discomfort. Here are a few clinical symptoms that must be assessed during a clinical review:
- Pain that is felt with the first steps in the morning is usually considered a strong factor in making the clinical diagnosis of plantar fasciitis;
- Plantar fasciitis pain and stiffness resolves with activity. On the contrary, tibial nerve entrapment (Tarsal tunnel syndrome) pain and calcaneal stress fracture pain are worsened with walking;
- Plantar fascia tenderness is truly at its worst toward the end of the day;
- Bilateral plantar fasciitis is reported in approximately 30% cases; and,
- Plantar fasciitis patients do not usually report night pain or feelings of and pins & needles. Presence of these two suggest other causes of heel pain such as neuralgia or neuropathies, tumors, tarsal tunnel syndrome and infections.
Examination and Clinical Tests:
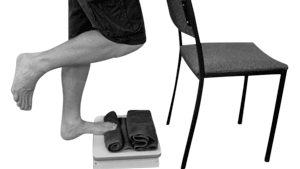
Windlass Test
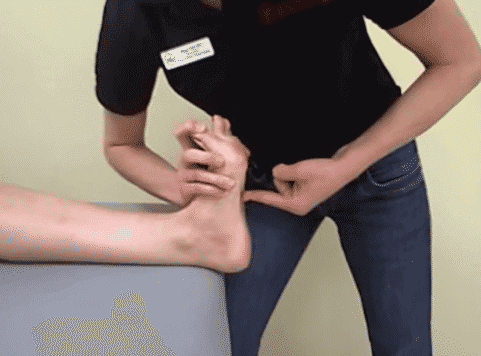
The test is positive if the patient’s pain is reproduced. Some versions of the test extend the big toe with one had while pressing on the plantar fascia with the other hand. To see a video of the non-weight bearing Windlass test, click here. For the weight-bearing test, the patient stands on step stool, equal weight on both feet with the toes just over the edge of the stool. The examiner stabilizes the ankle with one hand and with the other hand extends the big toe while flexing the flexing the interphalangeal joint i.e. extending the first metatarsophalangeal joint while allowing the interphalangeal joint to flex.The see a video of the weight bearing Windlass test, click here. For the weight-bearing test, the patient stands on step stool, equal weight on both feet with the toes just over the edge of the stool. The examiner stabilizes the ankle with one hand and with the other hand extends the big toe while flexing the flexing the interphalangeal joint i.e. extending the first metatarsophalangeal joint while allowing the interphalangeal joint to flex.The see a video of the weight bearing Windlass test, CLICK HERE
Heel Squeeze Test

Tinel’s Sign Test

This test rules out Tarsal Tunnel Syndrome. Tap along the inside ankle and a negative test is one where the tapping doesn’t produce any pain. A positive test is when tapping reproduces the pain and numbness which often radiate to the bottom of the heel. To see a video of Tinel’s sign, click here.
Diagnostic Tests:
Diagnostic tests (like radiology/ MRI) are usually not needed in making the diagnosis of plantar fasciitis, because, a complete history and physical examination helps in successfully making the diagnosis of plantar fasciitis in 95% of cases.
X-Ray Examination
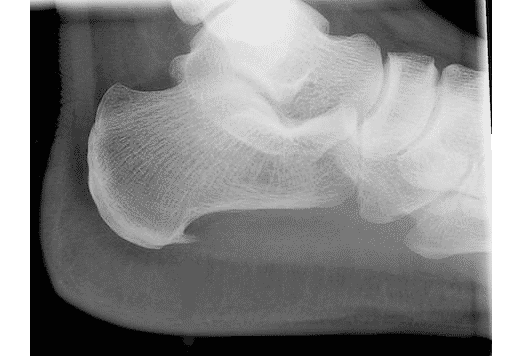
An x-ray is generally not indicated in making the diagnosis of plantar fasciitis. However, X-rays are frequently done since they are simple and help in the overall evaluation of the foot. An x-ray should be performed when: there is a history of unusual symptoms; in situations when patient symptoms do not improve (and/ or get worsen); and, when there is a risk of a coexisting condition, injury or disorder that may contribute to heel pain.
An x-ray may show a pronated foot type, which has been shown to correlate with chronic foot pain. Bone overgrowth or a bony spur is shown on the x-ray as a forward projection from the heel bone. Bony spurs may be be associated with plantar fasciitis pain. About 50% of patients with plantar fasciitis have bone spurs on x-ray and about 81% of all cases of bony spurs are symptomatic or associated with plantar fasciitis.
Ultrasound

Ultrasound examination is an excellent diagnostic tool for plantar fasciitis involves no exposure to radiation and is thought to be as effective or even more effective than an MRI or bone scan in diagnosing plantar fasciitis.
Ultrasound findings of plantar fasciitis include thickening of fascia (>4mm) observed as a darkened (hypoechoic) region, formation of osteophytes (heel spurs) and occasional calcification around the soft tissues of heel.
Other observations include soft tissue edema in the plantar heel as well as fat pad edema and degeneration. US is a useful imaging modality in the management of Plantar fasciitis since it is commonly used for the response to treatment and overall assessment of plantar fasciitis. Plantar fascia thickness diminishes on ultrasound with successful treatment.
MRI Scan
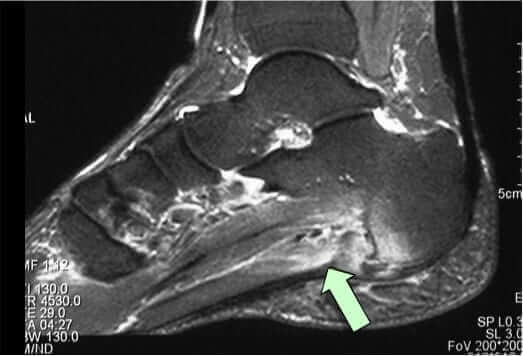
- Generalized thickening of plantar fascia (anything exceeding 4mm is considered abnormal)
- Increase in the signal intensity in the substance of the plantar fascia
MRI’s can also identify Plantar Fascia rupture, Achilles tendonitis, retrocalcaneal bursitis, calcaneal apophysitis, calcaneal stress fractures among other conditions.
Diagnostics Tests for Ruling Out Other Causes of Heel Pain:
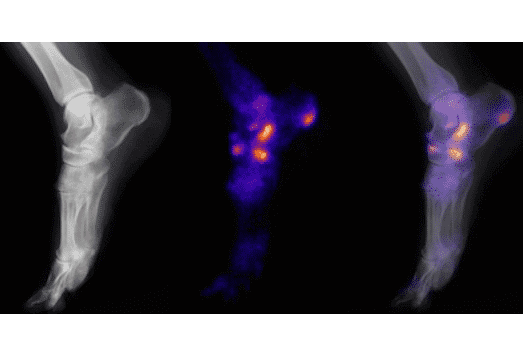
Bone Scan:
Bone scan is needed only to rule out other causes of heel pain. Specifically, a triphasic bone scan is often considered helpful in ruling out a calcaneal stress fracture, which may not appear in an conventional x-ray or MRI.

EMG (or Electromyogram):
EMG is used to rule out heel pain due to peripheral neuropathy and they can show nerve entrapment syndromes such as out Tarsal tunnel syndrome or other nerve entrapments.
Other tests
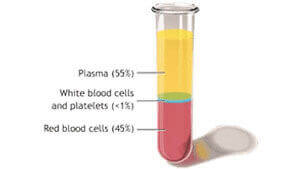
When there is bilateral heel pain or when symptoms do not improve (and/ or get worsen) despite conventional treatment blood tests should be ordered and these should include a complete blood count, erythrocyte sedimentation rate and a connective tissue disease screen.
Differential Diagnosis
There are a number of neurological and musculoskeletal conditions which can mimic the symptoms of plantar fasciitis and incorrect diagnosis can delay correct treatment.
- Tarsal tunnel syndrome: Tarsal Tunnel Syndrome (also referred to as posterior tibial neuralgia) is caused by an impingement or entrapment of the posterior Tibial nerve as it passes along the inside of your ankle. Patients with Tarsal Tunnel Syndrome report burning, tingling or numbness on the bottom of their foot (the plantar region) and have a positive Tinel’s sign without pain during passive upwards bending of the ankle (passive dorsiflexion.) See above. Patients with plantar fasciitis generally do not have burning, tingling or numbness but do have pain when their ankle is bent upwards.
- Other nerve entrapments: Entrapment of the first branch of the lateral plantar nerve (Baxter nerve) or the medial calcaneal branch of the tibial nerve can both present with symptoms very similar to plantar fasciitis and it can be quite difficult to distinguish between these. However nerve entrapments usually produce burning and tingling pain while plantar fasciitis does not
- Peripheral Neuropathy: The most common cause of peripheral neuropathy is chronic, poorly managed diabetes or alcohol abuse. The classic differentiating symptoms are: altered sensation on the bottom of the foot (the plantar region), a feeling of pins and needles, diffuse foot pain and no change in symptoms with weight bearing activities. Most patients with peripheral neuropathy also experience night pain or discomfort.
- L5-S1 radiculopathy: Bone or disk changes in the back can cause an irritation of the spinal nerve root, which supplies feeling to the foot. The irritated nerve can cause pain, numbness and/or tingling sensations which can radiate down the leg into the bottom of the foot. Other possible signs of lumbar radiculopathy are changes in sensation, reflexes or even muscle weakness. If you have pain in the foot in the leg or foot, you should call your doctor immediately and go to your local Emergency Room.
- Acute calcaneal fracture: Patients with fracture of calcaneus (the heel bone) can present with similar symptoms but with a clear history of fall or traumatic injury on the heel of the involved foot.
- Calcaneal stress fracture: Stress fractures of calcaneus (the heel bone) are seen very frequently in professional athletes or runners and are marked by diffuse swelling and warmth of the hind foot. Compression of the calcaneus (i.e., the squeeze test – see above) evokes pain in the heel that helps in making the diagnosis.
- Sever’s disease: Sever’s disease which is also referred to as calcaneal apophysitis is not a real disease but a painful inflammation of the heel’s growth plate typically affecting children between the ages of 8 and 14. It is seen in kids with an open growth plate (or “open physes”). This pain frequently doesn’t improve with walking. In Sever’s disease, heel pain is reproduced with squeezing the back of the heel.
- Systemic arthritis: Different types of arthritis including osteoarthritis in which multiple joints of the body are involved can present with heel pain and discomfort. Sometimes these can be related to connective tissue diseases such as rheumatologic disorders, Reiter’s disease, ankylosing spondylitis or psoriatic arthritis.
- Plantar Fat pad atrophy: This condition is more common in elderly population. In this condition the heel pad feels characteristically flattened and thinned with pain along the atrophied tissue. Although this can be detected by ultrasound the level of atrophy seen on ultrasound is not correlated with the level of pain or discomfort.
- Fat pad contusion: Bruising, contusion or traumatic damage to the heel fat pad is seen in fall or traumatic injuries that are associated with a hard landing on the ground. The pain is usually centered at the more towards the base of the heel than plantar fasciitis pain.
- Achilles tendinitis: Achilles tendinitis is marked by tenderness and pain along the back of the heel bone where the Achilles tendon inserts. The Achilles tendon is the largest tendon in the body. It connects your calf muscles to your heel bone and is used when you walk, run, and jump. Although the Achilles tendon can withstand great stresses from running and jumping, it is also prone to tendinitis, a condition associated with overuse and degeneration.
- Retrocalcaneal bursitis: This bursitis of the heel is swelling of the fluid-filled sac (bursa) at the back of the heel bone under the Achilles tendon causing stiffness and pain. Repeated or too much use of the ankle can cause this bursa to become irritated and inflamed. Possible causes are too much walking, running, or jumping. This condition is usually linked to and may be mistaken for Achilles tendinitis.
- Posterior tibial tendonitis: Posterior tibial tendonitis is an uncommon problem of one of the tendons on the inner side of the ankle. Pain is usually just underneath the prominence of the inner ankle (the medial malleolus.)
- Flexor hallucis longus tendonitis: Flexor hallucis longus tendonitis is a condition characterized by damage to the tendon with subsequent degeneration and inflammation. It occurs more commonly in ballet dancers resulting in pain in the region of the inner ankle, which may travel down to the big toe. This condition can be diagnosed by eliciting pain with resisted bending of the great toe. In some cases this condition can be especially difficult to tell apart form plantar fasciitis and an MRI may be required to confirm the diagnosis.
- Plantar Fibromatosis: This is an uncommon non-malignant thickening of the feet’s deep connective tissue, or fascia. Nodules or cords start growing along tendons of the foot and eventually the cords thicken, the toes stiffen and bend, and walking becomes painful. This condition is marked by pain along the sole of the foot in addition to bumps that you can feel within the fascial substance.
- Rupture of the plantar fascia: In all such cases, the pain is usually severe and sudden in onset. Examination may show localized swelling and bruising and feeling the bottom of the foot may reveal a subtle collapse in the long arch of the foot with a clearly felt gap within the substance of the fascia. Most of these ruptures heal successfully with nonsurgical treatment involving immobilization and prolonged non–weight bearing.)
- Metabolic conditions such as sickle cell anemia, Paget disease of bone, vascular insufficiency, osteomalacia and bone tumors can also present with symptoms that mimic plantar fasciitis.