Non-surgical Treatments for Plantar Fasciitis
We provide the non-surgical interventions and procedures as the second line of treatment if conservative treatments and ultrasound guided corticosteroid injections fail to cure your plantar fasciitis. These are usually considered after 2-3 months of conservative treatment with little improvement of plantar fasciitis symptoms. Physicians highly recommend these procedures over surgery because:
- These interventions are associated with minimal risk of adverse effects as compared to surgery
- Post-procedure rehabilitation/ recovery period is generally short and pain-free
- At least 80% of patients experience complete resolution of symptoms (thus not requiring surgical intervention)
Tired of all those stretching and icing exercises?
The non-surgical treatments for resistant Plantar Fasciitis that we recommend and perform are:
Extracorporeal Shock Wave Therapy (ESWT)
 If conservative measures are unsuccessful at eliminating plantar fasciitis pain, Extracorporeal Shock Wave Therapy (ESWT) is considered an excellent next step. We use a type of ESWT called Extracorporeal Pulse Activation Technology or EPAT®). We provide it as a simple and excellent treatment of plantar fasciitis. Recently, EPAT has also been shown to be very effective when used in early plantar fasciitis.
If conservative measures are unsuccessful at eliminating plantar fasciitis pain, Extracorporeal Shock Wave Therapy (ESWT) is considered an excellent next step. We use a type of ESWT called Extracorporeal Pulse Activation Technology or EPAT®). We provide it as a simple and excellent treatment of plantar fasciitis. Recently, EPAT has also been shown to be very effective when used in early plantar fasciitis.
Extracorporeal Pulse Activation Technology uses high frequency sound waves that are directed at the most tender part of the heel to promote healing. EPAT offers fast recovery without the necessity of reduced weight bearing or immobilization. The short recovery time allows the patients to resume their daily living activities earlier.
It is estimated that extracorporeal shock wave therapy is effective in resolving greater than 70% of cases of chronic plantar fasciitis pain. Recent studies have shown that patients with heel spurs, edema or high pain scores respond better to EPAT.
The exact therapeutic mechanism of shock wave therapy still remains a topic of speculation despite extensive research. It is thought that sound waves damage tissues to induce microtrauma, which stimulates the healing process by attracting blood vessels and nutrients to the plantar fascia. These sound waves also inhibit pain receptors to achieve pain relief and persistent healing of chronic processes.
The Procedure. Our protocol for EPAT is a course of 3 treatments, each 2 weeks apart. The procedure is generally well tolerated when performed by trained technicians with minimal discomfort.
Side effects are rare especially when procedure is performed in expert hands. Side effects may include: bruising, post-procedure inflammation, discomfort, pain, swelling and tenderness (all of which usually resolve spontaneously.) Contraindications to extracorporeal shockwave therapy include: a positive history of hemophilia or other coagulopathies; malignancy; and open bone growth plates (physes.)
Relief: Many patients have pain relief immediately after EPAT. EPAT has a cumulative effect so repeating the procedure can be beneficial. The full effect of the course of 3 treatments may take up to 6 weeks after the last treatment.
Ultrasound Guided Radiofrequency Ablation (RFA)
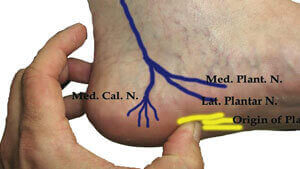
The mechanism of Plantar Fasciitis pain is unclear. In some cases, the cause of ongoing Plantar Fasciitis pain is that a sensory nerve to the heel (specifically a branch of the Inferior Calcaneal Nerve) is pinched between the heel and the overlying muscles due to the thickening of the plantar fascia. This results in a nerve entrapment syndrome called Baxter’s Entrapment. In these cases, permanently numbing the nerve’s pain sensation by using ultrasound guided radiofrequency ablation provides excellent long-term pain relief without any need for surgery.
 Ultrasound guided radiofrequency ablation is a sophisticated, minimally invasive procedure for Plantar Fasciitis. High patient satisfaction scores and long-term pain relief have been reported, especially for patients whose Plantar Fasciitis pain is due to Baxter’s Entrapment. The accuracy and precision of the procedure is significantly improved with the use of ultrasound and nerve stimulator guidance.
Ultrasound guided radiofrequency ablation is a sophisticated, minimally invasive procedure for Plantar Fasciitis. High patient satisfaction scores and long-term pain relief have been reported, especially for patients whose Plantar Fasciitis pain is due to Baxter’s Entrapment. The accuracy and precision of the procedure is significantly improved with the use of ultrasound and nerve stimulator guidance.
Radiofrequency ablation uses high frequency sound waves to heat the affected sensory nerve to 90 degrees Celsius. At this temperature, proteins in the nerve are broken down and the nerve is destroyed, which prevents the nerve fibers from transmitting pain from that area. Radiofrequency ablation can also stimulate the creation of new blood vessels, which accelerates the healing process. At our center, the intervention is performed
under local anesthesia and using nerve stimulator and ultrasound guidance to guarantee an accurate positioning. Most patients experience remarkable improvement in symptoms within a week after the procedure. The procedure has a therapeutic efficacy of over 80%. (The effects of the therapy may be lower in morbidly obese patients or patients with long complex histories.)
Diagnostic Injection: Ultrasound guided radiofrequency ablation is usually done after a diagnostic injection, which gives us an indication of the likely effectiveness of the ablation. A local anesthetic agent (such as lidocaine) is injected using nerve stimulator and ultrasound guidance to increase accuracy. If the trial injection results in a significant decrease in pain, then this indicates that the procedure is likely to be successful.
The Procedure: Radiofrequency ablation is mostly painless. You may feel pain only when the local anesthetic is injected into the foot. After the skin is anesthetized with local anesthetic, a very small puncture is made over the affected zone. The radiofrequency needle is introduced with the aid of ultrasound guidance and the positioning of the needle may be rechecked with a nerve stimulator. An electrode is then placed through the needle and heated according to the defined protocol. After the intervention, the treated area is covered with a bandage. The patient is advised to reduce activity, and to ice and elevate the foot for the remainder of the day. The bandage can be removed the following day and patient can cover the area with a regular Band-Aid, keeping the site dry and clean for at least 24 hours. Normal activity can be resumed within one or two days. Any pain that may occur can be managed with an NSAID or Tylenol.
Side effects: Radiofrequency ablation does not usually cause side effects, but a few are a possibility. Infections or abscess formation at the puncture site are rare. You may develop bruising that can be painful. Numbness or a lack of sensation in and around the incision area may also occur, but this a rare side effect.
Relief: It often takes 4-6 weeks for the full effect of the procedure. We recommend continued heel pads or arch supports as well as stretching for at least 2 months after the procedure. You should be able to resume physical activities such as jogging after one month. If pain persists after six weeks, the procedure can be repeated. If none of these procedures improve the pain, it may be time to look at other interventions. However, most patients report that after one or two radiofrequency ablations their Baxter’s entrapment pain has diminished significantly.
Ultrasound Guided Platelet Rich Plasma Injection
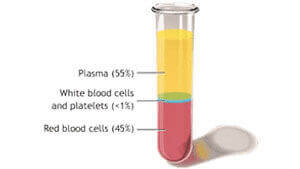
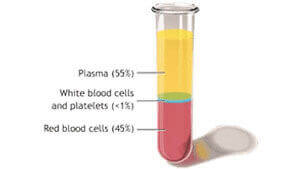
 Platelet rich plasma (PRP) treatment is the injection of the patient’s own platelets to jumpstart the healing process for soft tissue injuries such as injured tendons, ligaments, muscles, joints and plantar fasciitis.
The use of platelet-rich plasma injections for plantar fasciitis is relatively new. Recent studies have shown platelet-rich plasma injections to be effective in treating plantar fasciitis. Some studies even suggest that these injections should be adopted as the first line of treatment especially with recently developed injection techniques. Platelet activation plays a key role in the process of wound and soft tissue healing, especially when inflammation is present. Platelet-rich plasma injections are prepared by centrifuging the patient’s own blood to create a high concentration of platelets, around 7-10 times the concentration found in regular blood. These concentrated activated platelets are injected into the abnormal tissue, causing a local inflammatory reaction which releases growth factors that stimulate healing , tissue regeneration and accelerate recovery. The activated platelets also
Platelet rich plasma (PRP) treatment is the injection of the patient’s own platelets to jumpstart the healing process for soft tissue injuries such as injured tendons, ligaments, muscles, joints and plantar fasciitis.
The use of platelet-rich plasma injections for plantar fasciitis is relatively new. Recent studies have shown platelet-rich plasma injections to be effective in treating plantar fasciitis. Some studies even suggest that these injections should be adopted as the first line of treatment especially with recently developed injection techniques. Platelet activation plays a key role in the process of wound and soft tissue healing, especially when inflammation is present. Platelet-rich plasma injections are prepared by centrifuging the patient’s own blood to create a high concentration of platelets, around 7-10 times the concentration found in regular blood. These concentrated activated platelets are injected into the abnormal tissue, causing a local inflammatory reaction which releases growth factors that stimulate healing , tissue regeneration and accelerate recovery. The activated platelets also - Increase local blood flow to assist in correction of a failed healing response
- Induce a breakdown of scar tissue, which may have been produced as a result of a chronic inflammatory response.
 The use of ultrasound for the injection of platelet rich plasma increases the precision of injection and the quality of results while decreasing the likelihood of complications. PRP injection therapy is generally completed in just one session, but may require additional injections depending upon the clinical circumstances.
The use of ultrasound for the injection of platelet rich plasma increases the precision of injection and the quality of results while decreasing the likelihood of complications. PRP injection therapy is generally completed in just one session, but may require additional injections depending upon the clinical circumstances.
Since the procedure involves utilization of the patient’s own blood, the risk of adverse effects or complications is low. The procedure is generally well tolerated with high patient satisfaction scores and long term pain relief. Some side effects of platelet rich plasma injections are post-injection swelling and localized discomfort that usually goes away in a couple of days. Ice or over-the-counter analgesics (like Acetaminophen (Tylenol) but not NSAIDs) can help reduce discomfort after the procedure. Other less common risks of Platelet Rich Plasma injections include; infection, localized bruising or changes in skin color. PRP is contraindicated in breastfeeding/ pregnant women, individuals with known history of coagulation or bleeding disorders and malignant lesions. NSAIDs such as ibuprofen cannot be used after Platelet Rich Plasma injections since they interfere with the effectiveness of the PRP treatment.
Besides the management of plantar fasciitis, ultrasound guided platelet rich plasma injections can be used for the treatment of several other musculoskeletal conditions, such as tendonitis, sprains or strains to ligaments or articulating surfaces and muscle tears.
Other recommendations include:
The use of ultrasound guided Botulinum Toxin A (Botox) Injections to treat plantar fasciitis is considered highly experimental. It is generally well-tolerated, with high patient satisfaction scores and considerable symptomatic relief for a period of up to 3 months. Usually a dose of up to 200 units of botulinum toxin A is injected in two divided doses under ultrasound guidance. Botulinum toxin injection is not often used as a long-term management tool since the effects of botulinum toxin fade over time. Recent studies(5) have shown that Botox is not as effective as ESWT for the treatment of Plantar Fasciitis and so we discourage its use. It is not yet clear whether treatment of chronic plantar fasciitis with botulinum toxin A works by causing impaired movement of the muscle (paresis) or by analgesic/anti-inflammatory effects, or both. Besides plantar fasciitis, botulinum injections have been successfully used for the management of several musculoskeletal and neurological conditions.
Low-level laser therapy is a new and experimental modality used for the treatment of Plantar Fasciitis. The mechanism of action is unknown but early studies investigating the molecular effects of LLLT have focused on the photo biomodulation and photobiostimulation phenomena, which promote cell proliferation and tissue regeneration. A number of early studies showed that LLT was ineffective in treating Plantar Fasciitis but more recent studies have shown some effectiveness. In general, we feel that this treatment is still experimental and its effectiveness has not been clearly established.
This procedure is another highly experimental procedure for the treatment of Plantar fasciitis. Repeated corticosteroid injections are associated with a high rate of complications such as rupture of fascia, muscle or fat pad atrophy and degenerative damage to other tendons. However, a new and innovative procedure, Iontophoresis delivers corticosteroid to the fascia while reducing these complications. Iontophoresis involves the delivery of corticosteroid (0.4% dexamethasone) to the plantar fascia region without subjecting the patient to needles. As part of this procedure, two pad like electrodes are attached to the skin. Controlled quantities of electric current are produced across the electrodes, which drive the movement of chemicals (such as dexamethasone) across the skin without needing to insert any needles. This procedure is rarely used in the management of plantar fasciitis since the effectiveness of Iontophoresis is lower for deeper tissues (such as the plantar fascia) and the procedure is costly and time consuming. For instance, for effective pain relief the procedure must be performed 2-3 times per week.